Genetic Insights into Vegetable Consumption
sabeeh
on
August 12, 2024
Vegetable consumption transcends mere culinary practice; it is a cornerstone of a healthy and balanced dietary regimen. Let’s dive into the phytonutritional richness of vegetables, and their established role in promoting nutritional health and wellness, even disease prevention, explore their genetic influences, and find strategies to optimize vegetable consumption within the modern diet.
You may be interested in: New GWAS Study: Can Tendency For Vegetarianism Be Genetic?
Benefits of Plant-Based Diets
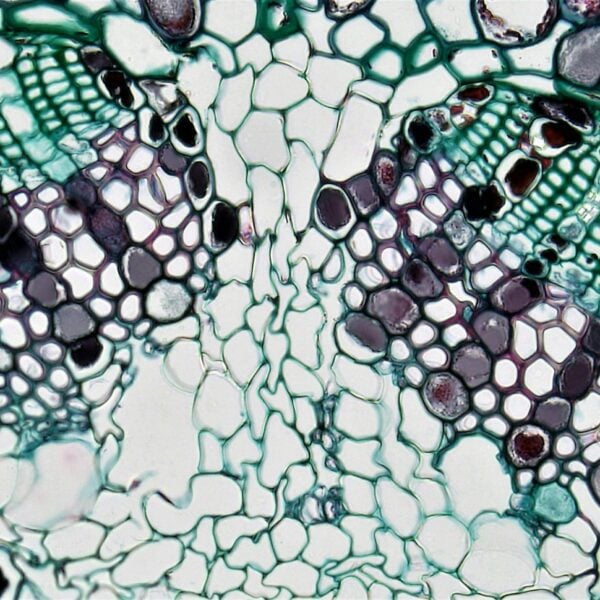
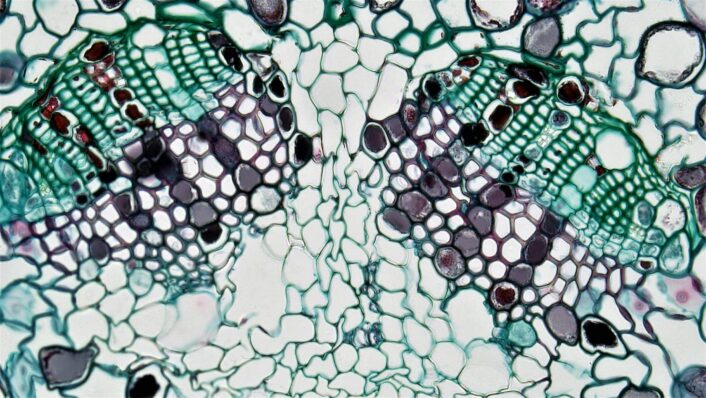
Extensive research underscores the significant health benefits associated with increased vegetable consumption. Studies have demonstrated a positive correlation between vegetable consumption and reduced risk of chronic diseases including cardiovascular disease, certain oncological manifestations, and type-2 diabetes mellitus. This protective effect can be attributed to the presence of a diverse array of bioactive compounds within vegetables.

Why Are Vegetables Good Sources of Nutrition?
Vegetables are a treasure trove of essential vitamins, minerals, and dietary fiber. They are abundant sources of essential micronutrients like vitamin A; crucial for ocular health, and potassium which plays a vital role in regulating blood pressure.
Additionally, vegetables are a significant source of dietary fiber, which promotes satiety, regulates digestion, and may contribute to weight management.
How Genetics May Influence Vegetable Consumption
Gene variations can play a significant role in determining individuals’ preferences and aversions towards certain foods, including vegetables. Here, we discuss the influence of specific genes on vegetable consumption, namely ORO10A2, TAS2R38, and CA6.
OR10A2
Research suggests that genetic variations in olfactory receptor genes, such as OR10A2, may influence the perception of certain odors associated with vegetables. For instance, a study identified a single-nucleotide polymorphism (SNP), rs72921001 in the OR10A2 gene that was significantly associated with the perception of a soapy taste in cilantro. This genetic association could explain why some individuals find cilantro unpleasant, as certain aldehydes present in cilantro interact with specific olfactory receptors, leading to variations in how people perceive its taste and aroma.
TAS2R38
The TAS2R38 gene encodes a bitter taste receptor and has been linked to individual differences in bitterness perception, particularly in most Brassica vegetables (e.g., broccoli, Brussels sprouts). Variations in three highly linked SNPs of the TAS2R38 gene (e.g. rs713598) give rise to two common haplotypes: PAV and AVI, which correlate with differences in bitter taste sensitivity. Studies have shown that individuals with certain TAS2R38 haplotypes may exhibit varying preferences for bitter-tasting foods and drinks, influencing their consumption patterns. For example, individuals with the AVI/AVI diplotype may consume coffee more frequently compared to those with the PAV/PAV diplotype.
You may be interested in: The Genetics of Bitter Taste Perception
CA6
Another gene, CA6, which encodes carbonic anhydrase VI (CA6), also plays a role in bitterness perception. An SNP within the CA6 gene, rs2274333, correlates with differences in bitterness sensitivity and has been associated with food choices that can determine health outcomes. Research suggests that carriers of the A-allele of the CA6 SNP may exhibit preferences for certain bitter-tasting food items, such as coffee, and this genetic predisposition could influence their overall dietary habits and potentially impact health parameters such as lipid profile, glucose levels, and systemic inflammation.
In summary, genetic variations in OR10A2, TAS2R38, and CA6 genes can contribute to individual differences in vegetable consumption by influencing taste perception and preferences. Understanding the genetic basis of food preferences can provide insights into dietary behaviors and may have implications for personalized nutrition and health interventions.
Non-Genetic Factors Influencing Vegetable Consumption
Vegetable consumption is a complex behavior influenced by a dynamic interplay of factors. Understanding these influences is crucial for promoting increased vegetable consumption and reaping their nutritional value and associated health benefits. Here’s a breakdown of key categories:
Demographic Factors
- Age: Studies suggest vegetable consumption tends to decrease with age.
- Gender: Some research indicates females may consume slightly more vegetables than males.
Environmental Factors
- Availability: Accessibility of fresh, affordable vegetables in supermarkets or local stores significantly impacts consumption.
- Seasonality: Seasonal variations in vegetable availability and price can influence choices.
Psychological Factors
- Taste Preferences: Dislike for certain vegetable flavors can be a hurdle.
- Knowledge and Attitudes: Understanding the health benefits and positive attitudes towards vegetables can promote consumption.
Behavioral Factors
- Cooking Skills and Habits: Limited cooking skills or lack of familiarity with vegetable preparation methods can be deterrents.
- Social Norms and Family Influences: Family dynamics, cultural norms, and social pressures can influence vegetable consumption habits.
Understanding these diverse factors is instrumental in developing effective strategies to increase vegetable consumption across different populations.
Strategies for Incorporating More Vegetables Into Your Diet
Despite the established wellness benefits, challenges persist in achieving optimal vegetable consumption within the contemporary diet. Here, we explore strategies to address these hurdles:
- Overcoming Palatability Barriers: Individuals with an aversion to raw vegetables may benefit from exploring alternative cooking methods such as roasting, grilling, or stir-frying, which enhance flavor profiles.
- Covert Veggie Integration: Pureed vegetables can be incorporated subtly into sauces, smoothies, or even baked goods, providing a discreet yet nutritious boost.
- Strategic Planning: Pre-cutting and prepping vegetables beforehand fosters convenient snacking and facilitates their inclusion within meals.
About the LifeDNA Nutrition Report
Discover the power of personalized nutrition with the LifeDNA Nutrition report! By analyzing your unique genetic profile, LifeDNA offers tailored recommendations to optimize your diet and well-being.
Gain insights into your vegetable consumption habits, so that you can ensure meeting your body’s specific nutritional needs. Take control of your well-being and unlock your full potential with LifeDNA. Start your journey to a better lifestyle today!
Summary
- Vegetables are rich sources of bioactive compounds linked to reduced risks of chronic diseases such as cardiovascular conditions, certain cancers, and type-2 diabetes.
- Vegetables offer essential vitamins, minerals, and fiber vital for health, including vitamin A for eye health and potassium for blood pressure regulation. Fiber also aids in satiety and digestion.
- Genetic variations in genes like OR10A2, TAS2R38, and CA6 can influence individuals’ preferences and aversions toward vegetables, particularly those with perceived unpalatable bitter tastes. OR10A2 affects taste perception due to sensitivity to vegetable odors; TAS2R38 influences preferences for bitter-tasting vegetables like broccoli; and CA6 impacts preferences for bitter foods like coffee. These genetic predispositions may explain why some individuals find certain vegetables unpleasant and how they can influence their dietary habits and health outcomes.
- Various factors beyond genetics affect vegetable consumption, including demographics (like age and gender), environmental factors (such as availability and seasonality), psychological factors (like taste preferences and attitudes), and behavioral factors (such as cooking skills and social influences).
- Practical strategies include enhancing palatability through alternative cooking methods, discreetly incorporating pureed vegetables into meals, and strategic meal planning to facilitate easier inclusion of vegetables in daily diets.
References
- https://pubmed.ncbi.nlm.nih.gov/31267783/#:~:text=Abstract,the%20plate%20at%20each%20meal.
- https://www.betterhealth.vic.gov.au/health/healthyliving/fruit-and-vegetables
- https://flavourjournal.biomedcentral.com/articles/10.1186/2044-7248-1-22
- https://www.sciencedirect.com/science/article/abs/pii/S019566631630736X?via%3Dihub
- https://www.cdc.gov/nchs/products/databriefs/db391.htm#:~:text=The%20percentage%20who%20consumed%20starchy,of%20adolescents%20aged%2012%E2%80%9319.
- https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-3-22#:~:text=Socio%2Ddemographic%20factors-,Gender,and%2For%20vegetables%20than%20boys.
- https://www.thewellnesscoalition.org/fresh-healthy-foods-accessibility-in-local-areas-that-need-it-most/#:~:text=When%20there%20is%20no%20access,intake%2C%20which%20improves%20health%20outcomes.
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.