Onset of Male Voice Breaking and Genetics
harvey
on
March 31, 2024
Latest Posts
Table of Contents
Onset of Male Voice Breaking and Genetics
Date of Content: March 8, 2024
Written by: Harvey Talento
Reviewed by: Maarit Tiirikainen, PhD
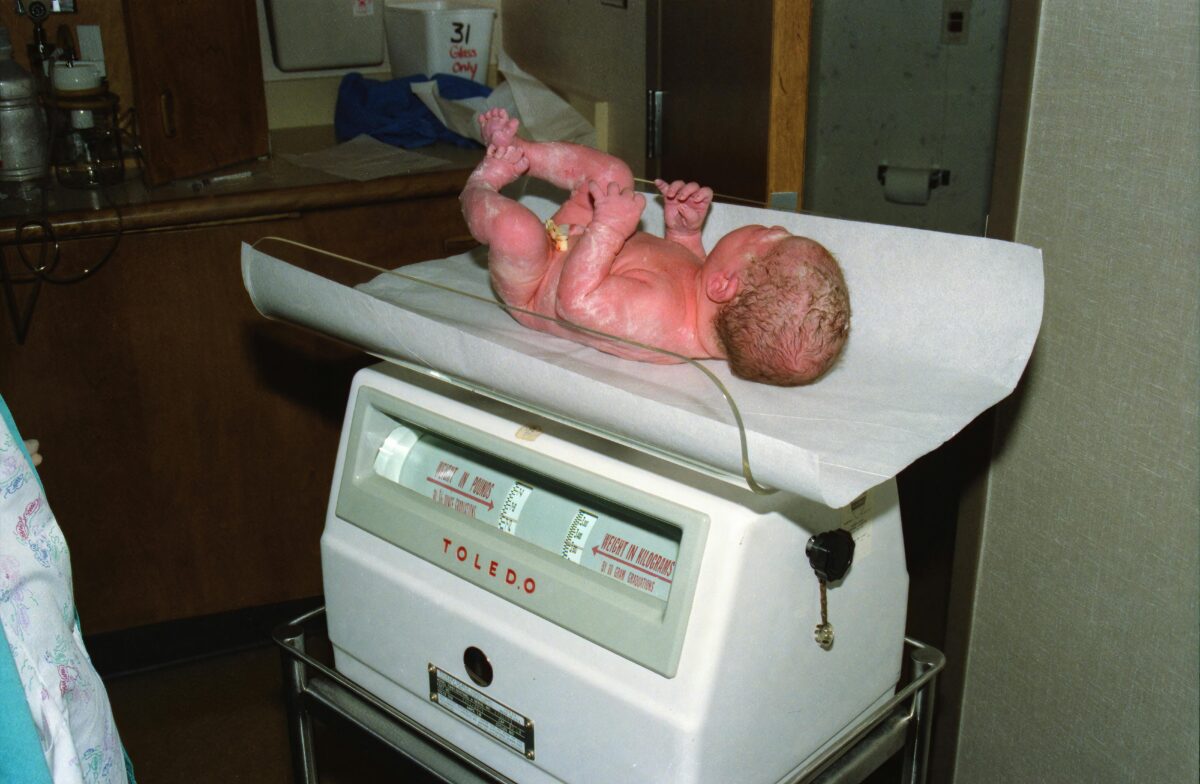
Adolescence is a period of remarkable changes, both physical and emotional. Among the most noticeable transformations for young men is the alteration of their voices.
This metamorphosis is a normal consequence of puberty, triggered by a growth spurt in the larynx, or voice box. A surge in testosterone levels fuels this development, causing the larynx to enlarge and the vocal folds to lengthen and thicken.

When Does A Boy’s Voice Change?
The timing of this transformation varies from individual to individual, but it typically occurs between the ages of 12 and 16, often following a period of rapid growth. Some young men experience a gradual deepening, while others endure a more dramatic shift punctuated by frequent voice cracks.
This phase, however, is impermanent, lasting only a few months. As the body adjusts to the hormonal fluctuations and the larynx stabilizes, the voice settles into its new, deeper register.
While the voice cracks can be a source of amusement (or perhaps frustration!), it’s crucial to remember that this is a natural and expected part of development. Embracing this change as a sign of maturation and remaining patient as the voice adjusts are key during this time.
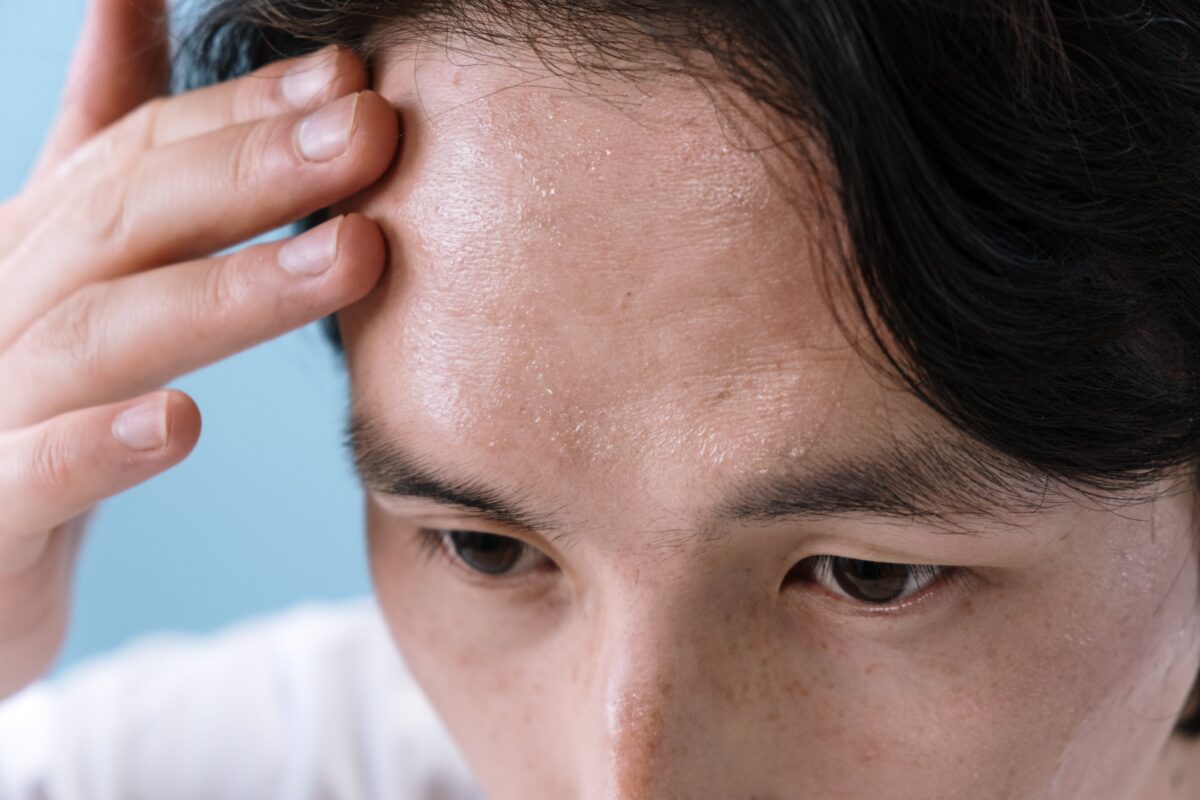
Does the Adam’s Apple Affect Voice Change?
While some researchers suggest that a larger Adam’s apple influences voice deepening and maturation, no concrete evidence to support this claim is available.
During puberty, the surge in testosterone stimulates the growth of the larynx, and the thyroid cartilage that forms the Adam’s apple becomes more prominent, particularly in males. This increased size is what creates the visible bump on the throat.
As mentioned, it is the growth of the larynx that plays a role in voice change. As the larynx gets bigger, the vocal folds (muscles within the larynx that vibrate to produce sound) also lengthen and thicken. A larger larynx and thicker vocal folds lead to a deeper vocal pitch in males.
In essence, the Adam’s apple becoming more prominent is a visible sign of the internal growth of the larynx, which can be linked to voice deepening. However, it’s important to reiterate that further research is needed to support this claim.
How Genetics May Influence the Onset of Male Voice Breaking
The onset of male voice breaking, a crucial event during puberty, is influenced by a combination of genetic and environmental factors. Several genes have been implicated in affecting the timing of male voice breaking, as identified through genetic studies such as genome-wide association studies (GWAS). Here are some key findings from a 2020 GWAS:
- LIN28B: LIN28B is involved in regulating the timing of puberty, and it may influence the onset of male voice breaking through its role in the maturation of various tissues and organs, including the larynx. It could affect the timing of hormonal changes that trigger vocal cord growth and changes in pitch. Genetic variation in SNP rs11156429 of this gene is associated with the onset of male voice breaking.
- KDM4C: This gene encodes a lysine-specific demethylase and may influence the onset of male voice breaking through its role in epigenetic regulation. Changes in gene expression controlled by KDM4C could affect the development of vocal cord tissues and their response to hormonal signals. SNP rs913588 in KDM4C is associated with later male voice breaking.
- ALX4: ALX4 is involved in fibroblast growth factor (FGF) signaling, which plays a crucial role in tissue development, including craniofacial and central nervous system (CNS) development. Genetic variation in SNP rs3824915 of ALX4 is associated with the onset of the male voice breaking.
- FGF11: This gene is involved in FGF signaling and CNS development. Changes in FGF11 expression or activity could influence the development of neural circuits involved in vocal control, potentially affecting voice modulation during puberty.
- TFAP4: TFAP4 encodes a transcription factor involved in gene regulation. It may influence the onset of male voice breaking by modulating the expression of genes involved in vocal cord development or hormone-signaling pathways that regulate puberty.
- SRD5A2: This gene encodes steroid 5-alpha-reductase, an enzyme involved in androgen metabolism. Changes in SRD5A2 activity could affect the metabolism of testosterone, a key hormone involved in voice deepening during puberty.
- LEPR: LEPR encodes the receptor for the hormone leptin, which regulates appetite and metabolism. Although its direct role in the onset of male voice breaking is unclear, leptin signaling may influence hormonal pathways involved in pubertal development, potentially impacting voice changes, and SNP rs2186245 in LEPR was found to be associated with the onset of male voice breaking.
- SMARCAD1, BDNF, FNDC9, FAM118A, ZNF446: These genes are involved in various biological processes such as chromatin remodeling, neurodevelopment, and transcriptional regulation. While their direct roles in the onset of male voice breaking are not well understood, alterations in their expression or activity could affect the development of vocal structures or hormonal pathways involved in puberty. Genetic variations in SNPs rs2049045 of BDNF and rs6006984 of FAM118A are associated with the onset of male voice breaking.
In summary, the onset of male voice breaking is influenced by a complex interplay of genetic factors, with multiple genes and biological pathways implicated in its regulation.
Non-Genetic Factors Influencing the Onset of Male Voice Breaking
While genetics play a major role in determining the timing of puberty and vocal changes, several non-genetic factors can influence the onset of male voice breaking. Here are some of the most well-researched ones:
- Nutrition: Good nutrition is essential for overall growth and development, including hormonal changes during puberty. A balanced diet rich in essential vitamins and minerals can support healthy vocal cord development and function.
- Overall Health: Chronic health conditions or illnesses can delay puberty and its associated changes, including the onset of male voice breaking.
- Weight: Being overweight or underweight can affect hormone levels and potentially influence the timing of puberty and voice changes.
- Endocrine Disruptions: Exposure to environmental toxins or endocrine disruptors can interfere with hormonal balance and potentially impact pubertal development.
- Socioeconomic Status: Studies suggest a link between socioeconomic factors and the timing of puberty. Generally, children from higher socioeconomic backgrounds may experience puberty slightly earlier than those from lower socioeconomic backgrounds. This could be due to various factors, including nutrition and overall wellness.
What To Do When Your Voice Starts Cracking
Below are some practical tips for managing voice changes during puberty.
Hydration
- Drink plenty of water throughout the day. This keeps your vocal cords lubricated and helps them function smoothly, reducing the risk of cracking or strain.
Vocal Hygiene
- Avoid yelling, screaming, or straining your voice. This can irritate your vocal cords and worsen voice cracks.
- Get enough sleep. When you’re well-rested, your voice is more likely to be strong and clear.
- Avoid smoking and second-hand smoke. Smoking irritates the vocal cords and can contribute to voice problems.
Vocal Warm-ups (Optional)
- Simple vocal warm-ups can help prepare your voice for speaking or singing. Humming, lip trills, and gentle scales can help improve vocal cord flexibility and reduce strain.
Communication Strategies
- Be patient with yourself! Voice changes take time to adjust to.
- Speak clearly and at a moderate volume. Don’t force your voice to sound lower than it naturally is.
- If you’re giving a presentation or participating in a play, practice beforehand to get comfortable with your new voice.
- If your voice cracks, don’t panic. Just take a deep breath and start again. Most people won’t even notice.
About the LifeDNA Wellness Report
Understanding even complex factors like the Onset of Male Voice Breaking becomes pivotal as we navigate the intricate pathways of our well-being. Imagine having personalized insights into your unique genetic traits related to your wellness. This is where the LifeDNA Wellness Report steps in. Going beyond generic advice, this tool provides tailored recommendations based on your genetic code, offering a holistic perspective on your well-being. By unlocking your genetic insights, you can take proactive steps towards a brighter, more informed lifestyle with the LifeDNA Wellness Report. Get it today!
Summary
- Puberty triggers voice changes in adolescent boys, driven by a surge in testosterone that enlarges the larynx and thickens vocal folds, typically occurring between ages 12 and 16.
- Although some suggest a correlation, evidence linking Adam’s apple size to voice deepening is inconclusive. Testosterone-induced larynx growth primarily drives voice changes during puberty.
- Genetic and environmental factors influence the onset of male voice breaking, with genes like LIN28B, KDM4C, ALX4, FGF11, TFAP4, SRD5A2, LEPR, and others implicated in puberty timing and hormone signaling.
- Nutrition, overall health, weight, endocrine disruptors, and socioeconomic status impact puberty timing, emphasizing the importance of balanced nutrition, health, and avoidance of endocrine disruptors.
- Hydration, vocal hygiene, proper sleep, avoiding smoking, and practicing vocal warm-ups support vocal health. Patience, clear communication, and strategies for presentations help manage voice changes gracefully.
References
- https://health.clevelandclinic.org/voice-changes-what-can-they-tell-you-as-you-age
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/talking-with-children-about-puberty
- https://my.clevelandclinic.org/health/body/24656-adams-apple
- https://www.nature.com/articles/s41467-020-14451-5
- https://www.researchgate.net/publication/268517133_Nutrition_and_pubertal_development
- https://pubmed.ncbi.nlm.nih.gov/11987900/
- https://joe.bioscientifica.com/view/journals/joe/218/2/R1.xml
- https://karger.com/hrp/article/93/9-10/548/167236/Socioeconomic-Status-Is-Related-to-Pubertal
Customer Reviews




*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports and suggestions do not diagnose or treat any health conditions or provide any medical advice. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results.