GeneFood: Everything You Need To Know
Aira
on
February 23, 2024
Latest Posts
Table of Contents
GeneFood: Everything You Need To Know
Date of Content: January 20, 2024
Written by: Avanthika Nityanand
Reviewed by: Maarit Tiirikainen, Ph
About GeneFood
Gene Food, led by Dr. Aaron Gardner, emphasizes a science-first approach to personalized nutrition. The company spent its first two years reviewing genetic and nutrition studies to develop a custom nutrition plan. Their proprietary algorithm categorizes individuals into one of twenty diet types based on over 120 genetic factors.
Since 2018, Gene Food has utilized genetic data from various providers to offer personalized nutrition advice, aiming to understand individual responses to dietary fats and other nutrition-related queries.

Services
Individuals can order a DNA Test Kit or upload existing raw genetic data from platforms like 23andMe to receive a personalized diet plan, including a Keto Score.
The analysis focuses on genes related to the metabolism of fats, proteins, and carbohydrates, as well as genetic markers for MTHFR, histamine, sulfur, ApoE4, and tolerances to lactose and wheat. This comprehensive evaluation forms the basis for a customized diet and nutrition strategy tailored to genetic profiles.
Pricing
Gene Food offers various services for personalized nutrition based on genetic data.
For $95, users can upload raw DNA data from providers like Ancestry, 23andMe, or MyHeritage to receive a diet type, health reports, and food sensitivity analysis, with results in 5 minutes and options for upgrades.
The $249 DNA Test package provides a more comprehensive analysis with additional genes for a complete score.
For an annual fee of $99, the Health Intelligence service updates users with new genes, health reports, and access to premium content, enhancing their understanding of personal health genomics.
For 23andMe Users
The approach involves uploading the raw genetic data from platforms like 23andme or Ancestry. This data is then analyzed to assess various genetic markers related to metabolism, tolerance to certain foods, and sleep patterns.
The report is a comprehensive nutrition plan that includes a unique diet tailored to the genetic makeup. It also offers insights into optimal fat, carbohydrate, and protein ratios, as well as personalized advice on managing LDL cholesterol, micronutrient supplementation, and dietary preferences.
Additionally, the plan explores one’s potential for achieving nutritional ketosis, responses to saturated fat, and the viability of a plant-based keto diet, complemented by tools and tests for further personalization. It also delves into sleep chronotypes, suggesting ideal sleep schedules and productivity timings, alongside an analysis of caffeine metabolism.
List of traits:
Your Unique Diet Type
Learn the ideal ratio of fat, carbs, and protein
LDL scoring and cholesterol absorption
Micronutrients and Supplements
Histamine, Dairy, Wheat, and much more
Your Ketogenic Diet Score
Can you achieve nutritional ketosis?
Saturated fat response
Is plant-based keto an option?
Keto tools and tests
Your Sleep Chronotype
Learn your ideal bedtime
Best time of day for productivity
Sleep genetics
Caffeine metabolism
Diet Types
Gene Food employs a proprietary algorithm to map individuals to one of twenty unique diet types based on an analysis of over 120 carefully selected genetic markers. This system personalizes nutrition recommendations, accommodating various dietary preferences and health objectives. These diet types are inspired by several factors, including geographical influences, modern diet research, and ancestral eating patterns, offering a tailored approach to nutrition. Gene Food’s services include DNA testing kits and the evaluation of genetic information from other providers, allowing for a comprehensive dietary planning tool.
Privacy
The company prioritizes the protection of genetic data, emphasizing privacy and security. Their genetics web applications are hosted on Amazon Web Services (AWS), known for its robust security protocols. The genetics laboratory in Houston, Texas, complies with the Clinical Laboratory Improvement Amendments (CLIA) to ensure high-quality lab testing. The company strictly adheres to privacy standards, never sharing data with third parties and using the provided data solely for delivering personalized nutrition and health insights.
Alternative to GeneFood: Why LifeDNA?
LifeDNA has emerged as a prominent option for analyzing 23andMe and many other raw DNA data sources, owing to a combination of unique offerings and a commitment to personalized wellness via our comprehensive set of multiple Reports addressing several different aspects of your overall well-being.
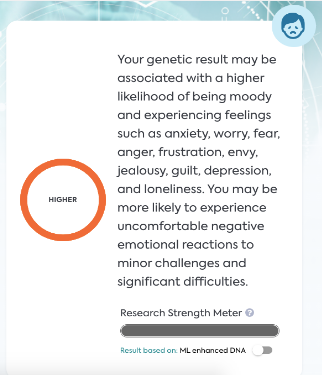
We offer a basic DNA raw data analysis package to kickstart your journey. Users with raw data from 23andMe, AncestryDNA, etc., can access 194+ traits across interests such as Nutrition, Wellness, Vitamins and Supplements, Personality, Fitness, Sleep, Methylation, and Skincare.
Further, if you do not have raw DNA data, such as from 23andMe, LifeDNA provides that too. Start your personalized wellness journey with LifeDNA’s state-of-the-art DNA kits here.
Here is why many regard LifeDNA as the best option for making the most of your 23andMe, AncestryDNA, and other raw data:
- Holistic Approach to Wellness: Unlike many other platforms that focus strictly on health-related risks or ancestry, LifeDNA adopts a holistic approach. We analyze genetic data to offer personalized optimizations for nutrition (including a customized grocery list!), skin care, vitamins & supplements, wellness, personality & cognition, and fitness. This range lets users get a complete picture of their wellness needs based on their DNA.
- Product Recommendations: We go beyond just providing insights. We offer specific product recommendations, skincare ingredients, or supplements tailored to an individual’s genetic profile. It makes our service actionable, allowing users to make immediate changes based on their results.
- Data Security: At LifeDNA, we highly emphasize protecting user data. Our commitment to privacy ensures that users can trust the platform with their sensitive genetic information.
- User-Friendly Reports: LifeDNA reports are easy to interpret. Our reports are designed to be accessible to the layperson without compromising on the depth and accuracy of the information.
- Continual Updates: As genetic research evolves, so does LifeDNA’s platform. Users can expect their reports and insights to be updated with the latest scientific findings.
- Dedicated Research and Development: At LifeDNA, we invest in research to continually refine our algorithms, ensuring that the insights provided are based on cutting-edge science.
- Educational Resources: LifeDNA also provides ample resources for users to understand their genetic makeup better. This education-first approach demystifies the complex world of genetics, making it approachable and actionable for everyone.
- Scientific rigor: To create an unmatched commitment to scientific rigor, LifeDNA partners with CLIA-certified, CAP-accredited, and HIPAA-compliant laboratories.
Customer Reviews




*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.