How Do Genes Influence Your Vitamin B5 Needs?
Aira
on
December 1, 2023
Latest Posts
Table of Contents
How Do Genes Influence Your Vitamin B5 Needs?
Date of Content: November 13, 2023
Written by: Harvey Talento
Reviewed by: Maarit Tiirikainen, PhD
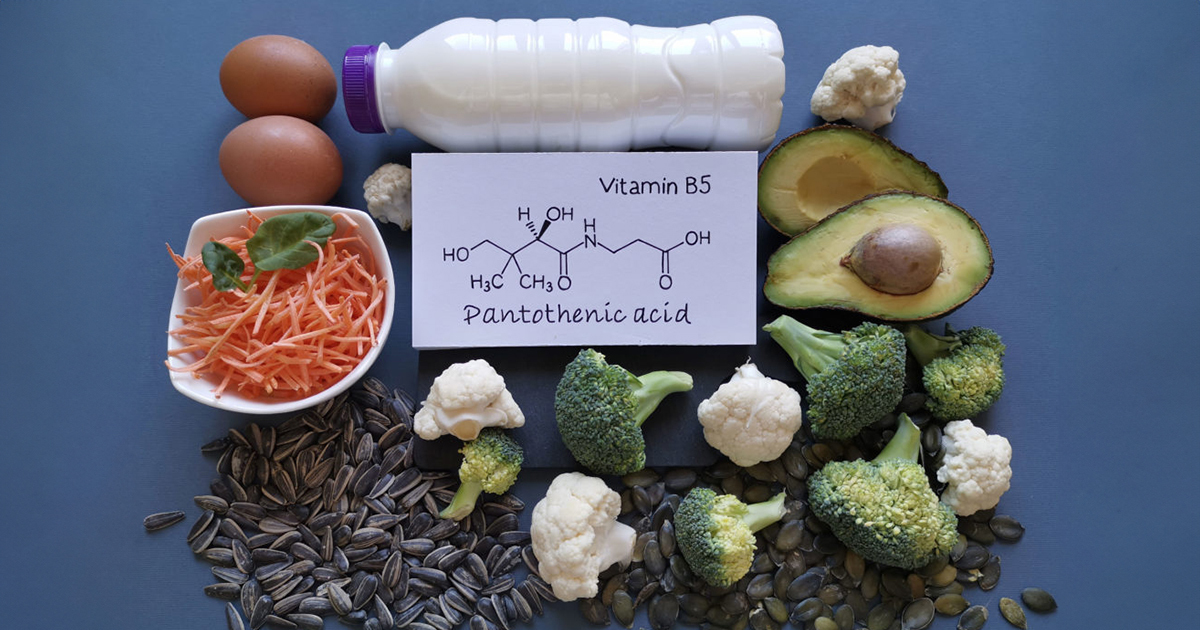
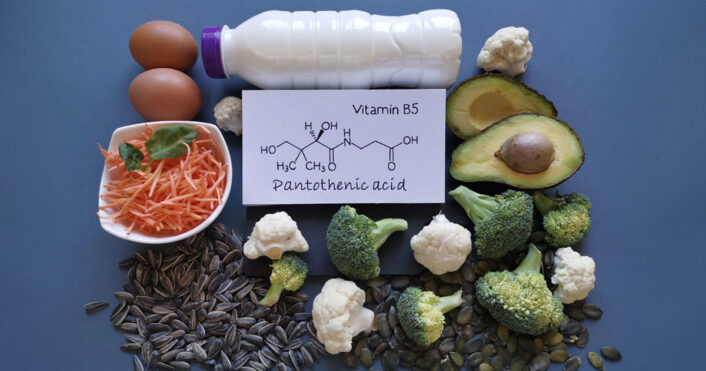
What is Vitamin B5?
Vitamin B5, also known as pantothenic acid, is an essential nutrient present in various foods and supplements. It supports the body in producing coenzyme A (CoA) and acyl carrier protein, crucial for tasks such as breaking down fats. During consumption, the majority of Vitamin B5 comes in diverse forms, but the body converts them into a straightforward form that is usable.
What Does Vitamin B5 Do to Your Body?
Vitamin B5 serves many essential functions in the body, contributing to overall wellness. Here are some key roles that vitamin B5 plays:
- Making Coenzyme A
Vitamin B5 plays a role in making coenzyme A, a key player in various metabolic pathways. Coenzyme A is instrumental in the synthesis of fatty acids, facilitating the conversion of dietary components into essential fats and cholesterol.
Additionally, it contributes to the production of sphingosine, a lipid-like molecule that functions in transmitting chemical messages within the body’s cells. Notably, the liver relies on coenzyme A to metabolize certain drugs and toxins safely.
- Supporting a Good Digestive System
Maintaining a good digestive system is crucial for overall well-being, directly impacting nutrient absorption and utilization. Vitamin B5 plays a significant role in this process, assisting in the use of other essential vitamins, especially vitamin B2.
The collaboration between these vitamins optimizes the efficiency of nutrient absorption, fostering optimal digestive function. Through its support for the digestive system, Vitamin B5 helps guarantee that the body can effectively extract and use nutrients, contributing to overall well-being and vitality.
- Skin Moisturization and Wound Healing
The importance of skin moisturization and efficient wound healing cannot be overstated. Vitamin B5 has demonstrated its efficacy in both these aspects. Studies indicate that Vitamin B5 serves as a potent moisturizer for the skin, promoting hydration and skin wellness.
Furthermore, research has shown promising results in using Vitamin B5 as a dietary supplement for facial acne, with a significant reduction in total lesion count over a 12-week period. While these findings are encouraging, further clinical trials are warranted to validate the results.
- Cholesterol and Triglyceride Regulation
Maintaining optimal cholesterol and triglyceride levels is crucial for cardiovascular wellness. Vitamin B5 has been implicated in potentially contributing to the regulation of cholesterol and blood triglyceride levels, as suggested by some studies.
However, it is imperative to highlight that any approach to managing cholesterol levels should only be undertaken under medical supervision. Vitamin B5’s potential role in this regard emphasizes the interconnectedness of nutrition and cardiovascular wellness, highlighting the need for a comprehensive and medically guided approach to address lipid profile imbalances.
The roles of vitamin B5 are crucial in maintaining overall well-being. Therefore, it is important to balance its levels in our bodies to keep us in top shape.
Genetics of Vitamin B5 Levels
Understanding the genetics of vitamin B5 levels holds the promise of personalized nutrition and targeted wellness interventions. By identifying specific genetic variations related to vitamin B5 metabolism, individuals can receive tailored dietary suggestions and interventions to optimize their nutrient levels.
The following are some genes that play a role in Vitamin B5 levels.
PANK 2
This gene encodes Pantothenate kinase 2, an enzyme that catalyzes the first step of vitamin B5 (pantothenic acid) metabolism, converting it to 4’-phosphopantothenic acid. This enzyme is inhibited by coenzyme A, a derivative of vitamin B5 that is essential for many biochemical reactions.
SLC5A6
The SLC5A6 gene provides instructions for making a protein called the sodium (Na+): multivitamin transporter (SMVT). This protein acts as a carrier that helps bring important vitamins, including vitamin B5, into our cells.
When there are changes in this gene, such as when the SNP rs1395 is present, it can influence the function of the SMVT protein. A study suggests that individuals carrying the A allele of rs1395 may experience variations in how their cells absorb and handle vitamin B5.
It is important to note that while information on genetic factors affecting vitamin B5 levels provides valuable insights, it is just one aspect of a holistic approach to wellness. Lifestyle factors, environmental influences, and overall wellness assessments should also be considered to comprehensively understand an individual’s well-being.
Non-Genetic Factors Influencing Vitamin B5 Levels
As we investigate the role of vitamin B5 in our bodies, it’s essential to recognize that genetic factors aren’t the sole influencers. External elements, such as diet, medications, stress, and age, play pivotal roles in shaping the intricate dynamics of vitamin B5 metabolism.
Diet
A diet that is low in vitamin B5 or high in processed foods that contain little or no vitamin B5 may lead to deficiency. Conversely, a diet that is rich in vitamin B5 or fortified with vitamin B5 may increase the levels of this vitamin in the body.
Medications
Some medications may interfere with the absorption or metabolism of vitamin B5, including antibiotics, oral contraceptives, anticonvulsants, and cholesterol-lowering drugs. These medications may reduce the levels of vitamin B5 in the body or increase the requirement for this vitamin.
Stress
Age
Age may affect the levels of vitamin B5 in the body, as older adults may have lower absorption and higher excretion of vitamin B5 compared to younger adults. Older adults may also have a lower intake of vitamin B5 from the diet or lower production of vitamin B5 by intestinal bacteria.
Keeping our vitamin B5 levels in balance is easier when we pay attention to how we treat our bodies. Being aware of our habits and surroundings helps us make choices that support good vitamin B5 levels, which is important for our overall well-being.
How to Optimize Vitamin B5 Levels Naturally
Exploring dietary avenues to optimize vitamin B5 levels naturally reveals a spectrum of nutrient-rich foods. The following are some items to consider:
Organ Meats
Among the most potent sources, organ meats (liver, kidney, and heart) deliver a substantial dose of vitamin B5, boasting up to 8.3 mg per 3 oz serving. Beyond vitamin B5, they are nutritional powerhouses, offering a symphony of other essential B vitamins, iron, and protein for overall bodily functions. Incorporating organ meats into your diet provides a comprehensive nutrient profile vital for optimal well-being.
Mushrooms
Mushrooms, particularly when dried, emerge as a concentrated source of vitamin B5, providing a remarkable 21.9 mg per 100 grams. Beyond their B5 content, mushrooms contribute vitamin D for the bones, selenium with antioxidant properties, and a medley of antioxidants that support overall immune function. Including a variety of mushrooms in your meals enhances flavor and enriches your diet with a diverse range of nutrients.
Sunflower Seeds
Enjoying sunflower seeds as a snack introduces a delightful way to boost your vitamin B5 intake, offering 6 mg per 3 oz serving. These seeds go beyond B5, providing vitamin E for the skin, magnesium for muscle and nerve function, and good fats contributing to cardiovascular well-being. Incorporating sunflower seeds into your diet satisfies your taste buds and nourishes your body with a blend of essential nutrients.
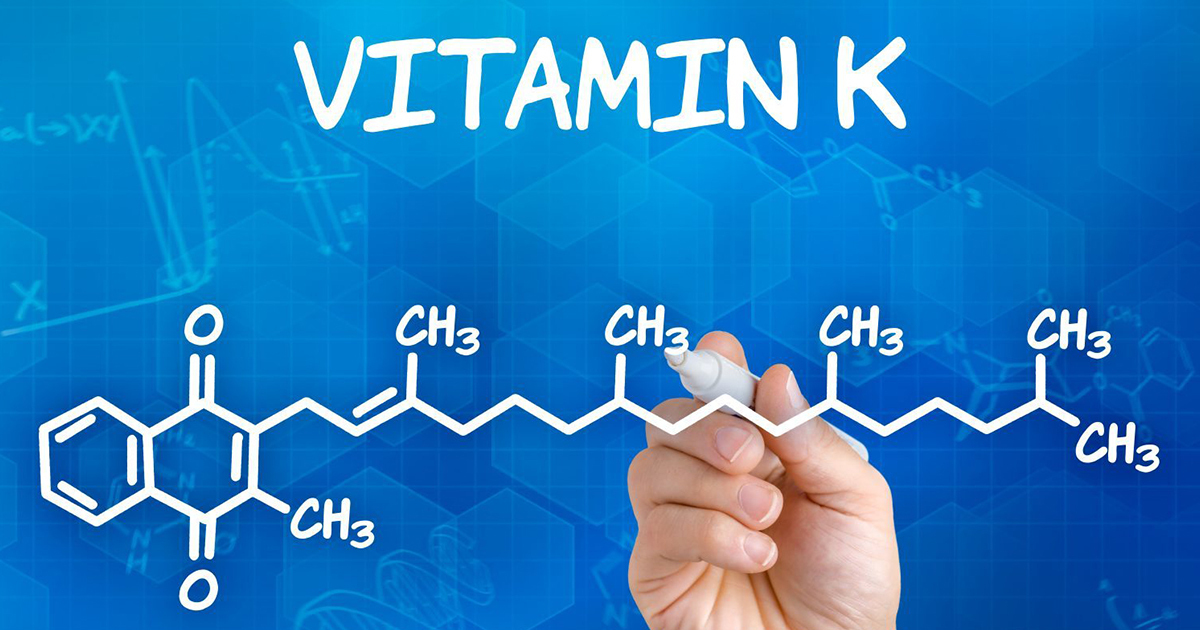
Avocados
Avocados, known for their creamy texture, contribute 2 mg of vitamin B5 per fruit. Alongside vitamin B5, avocados offer a rich array of nutrients, including vitamin K for blood clotting and the bones, folate crucial for cell division, potassium for heart wellness, and monounsaturated fats that support a good cardiovascular system. Integrating avocados into your meals adds a delicious and nutrient-dense element to promote overall wellness.
Salmon
Salmon, a fatty fish, provides 1.6 mg of vitamin B5 per 3 oz serving. Beyond vitamin B5, salmon is renowned for its omega-3 fatty acids; promoting heart wellness, vitamin B12 which is crucial for nerve function, and selenium which has antioxidant properties. Including salmon in your diet contributes to your B5 intake and delivers a bounty of essential nutrients that support various bodily functions, making it a valuable addition to a nutritious diet.
Other foods containing vitamin B5 include eggs, dairy products, whole grains, legumes, broccoli, and fortified cereals. While vitamin B5 supplements are available, obtaining nutrients from natural food sources is generally suggested.
Dietary Supplements
Vitamin B5 can also be taken through dietary supplements. These may contain only Vitamin B5, combined with other B-complex vitamins, or as part of some multivitamin/multimineral products.
About the LifeDNA Report
LifeDNA’s Vitamins & Supplements Report is your personalized roadmap for optimizing Vitamin B5 levels based on your unique genetic traits. This report delves into your genetic predispositions, offering tailored dietary recommendations to enhance your Vitamin B5 levels.
Uncover insights into your genetic tendencies related to Vitamin B5 levels, and take the first step toward achieving optimal wellness with the LifeDNA Vitamins & Supplements Report.
Start your journey to personalized well-being today!
Summary
- Vitamin B5, or pantothenic acid, crucial for many metabolic processes, is absorbed through active transport mechanisms and is found in both plant and animal food sources.
- Vitamin B5 supports coenzyme A synthesis which is needed for fatty acid and cholesterol production, aids digestion, and shows potential benefits on the skin and cholesterol regulation.
- The PANK2 gene initiates vitamin B5 metabolism.
- External factors such as diet, medications, stress, and age significantly impact vitamin B5 levels, emphasizing the importance of a balanced lifestyle.
- Dietary sources rich in vitamin B5, including organ meats, mushrooms, sunflower seeds, avocados, salmon, and various other foods, provide a holistic approach to maintaining optimal vitamin B5 levels for overall well-being.
References
- https://ods.od.nih.gov/factsheets/PantothenicAcid-HealthProfessional/
- https://lpi.oregonstate.edu/mic/vitamins/pantothenic-acid
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4065280/
- https://lpi.oregonstate.edu/mic/vitamins/pantothenic-acid
- https://lpi.oregonstate.edu/mic/vitamins/pantothenic-acid
- https://www.nature.com/articles/s41431-021-01033-2
- https://www.nature.com/articles/ng.2982
- https://www.frontiersin.org/articles/10.3389/fmed.2022.1089476/full
- https://www.frontiersin.org/articles/10.3389/fmed.2022.1089476/full#:~:text=4.1.%20B5%20vitamin%20(pantothenic%20acid)
- https://med.libretexts.org/Courses/American_River_College/General_Nutrition_Textbook_%28not_Plant-Based%29-_reference_for_NUTRI_303_%28Hagenburger%29/7%3A_Vitamins/7.3%3A_Water_Soluble_Vitamins/Vitamin_B5_%28Pantothenic_acid%29
- https://med.libretexts.org/Courses/American_River_College/General_Nutrition_Textbook_%28not_Plant-Based%29-_reference_for_NUTRI_303_%28Hagenburger%29/7%3A_Vitamins/7.3%3A_Water_Soluble_Vitamins/Vitamin_B5_%28Pantothenic_acid%29
- https://pubmed.ncbi.nlm.nih.gov/31691401/
- https://www.frontiersin.org/articles/10.3389/fnut.2019.00048/full
- https://med.libretexts.org/Courses/American_River_College/General_Nutrition_Textbook_%28not_Plant-Based%29-_reference_for_NUTRI_303_%28Hagenburger%29/7%3A_Vitamins/7.3%3A_Water_Soluble_Vitamins/Vitamin_B5_%28Pantothenic_acid%29
- https://www.hsph.harvard.edu/nutritionsource/pantothenic-acid-vitamin-b5/
Customer Reviews




*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.